Abstract
Introduction
Several reports have been published showing that T cell replete haploidentical stem cell transplantation (TCR-Haplo-SCT) with post-transplantation cyclophosphamide (PTCy) is feasible and achieves good results in children and young adults with hematologic malignancies, however most of them have included patients until 21 years, a variety of malignancies and the follow up informed have been short, indeed, only one described outcomes until 36 months. Here we present the long term follow up of 39 patients, < 18 years old, with high-risk leukemia, transplanted with TCR-Haplo-SCT and PTCy in one institution
Methods and Patients:
The cellular source was PBSC, the mobilization was done with filgrastim and the cells were collected with one apheresis procedure. Two conditioning were used: fludarabine 30 mg/m2/day for 5 days, oral busulfan 4-8 mg/kg/split in 1-2 days and total body irradiation 400 cGy on day - 1 (Flu Bu TBI) or fludarabine, same dose, melphalan 100-140 mg/m2, one day and TBI 200-400 cGy on day - 1 (Flu Mel TBI). The patients received PTCy 50 mg/kg/day on D+3 and D+4, followed by cyclosporine and oral mycophenolate starting on day + 5.
After a signed informed consent, 39 patients were transplanted. The diagnoses were: acute lymphoblastic leukemia (ALL): 22, acute myeloid leukemia (AML): 14, juvenile myelomonocytic leukemia (JMML): 2, blastic phase of chronic myeloid leukemia (CML blastic): 1. Eleven out of 39 (28%) were in first remission (CR1), 18/39 (46%) in second (CR2), and 10/39 (26%) in third or with refractory disease (CR3). The indication for transplantation of patients in CR1 was: JMML: 2 cases, ALL with high MRD levels after induction: 3, CML blastic: 1, AML without CR after induction: 4 or with complex karyotype: 1.
Median age was 7.6 years (range 2-17), 17 out of 39 were younger than 10 year s and, 18 were female.
Results:
All the donors shared 4 out of 8 alleles; in 61% of the cases the donor was the mother, in 26% the father and in 13% a sibling. 17 patients (38%) were given Flu Bu TBI and 22 (56%) received Flu Mel TBI.
A median of 14 million of CD34+ cells/kg was infused (range 7-38). For patients younger than 10 years the median was 17 million (range 7-38) and for older 12 million (range 8-19) P: 0.08. The engraftment rate in 38 patients alive at d+30 was 100%, median time to reach 500 neutrophil or more and a self- sustained platelet count of 20.000 was 14 days for both (range 12-20 and 8-48). Chimerism at day + 100 was available in 35 cases; all of them had full donor hematopoiesis.
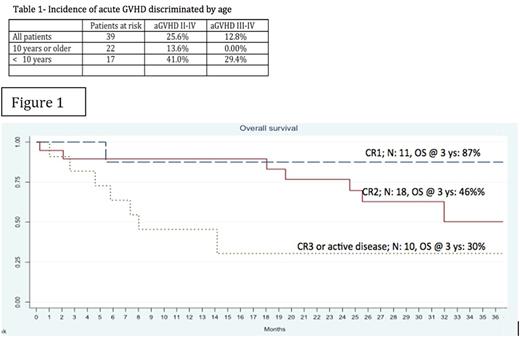
The median follow-up of the whole group was 20 months (range 3- 52), while for alive and deceased patients were 26 and 7.7 months respectively. The accumulative incidence of acute graft versus host disease (aGVHD) II-IV and III-IV was 25 and 13%, it was unexpected higher in patients younger than 10 years; indeed, all the severe cases belong to this group (Tab 1). The incidence of extensive chronic graft versus host disease was 16.6%
The overall relapsed rate was 23%, the transplant related mortality (TRM) at 1 year was 15.4%. The overall (OS) and event free survival (EFS) at 36 months (Kaplan Meier) for the whole group was 51 and 48%. When OS and EFS were discriminated by state of the disease, the results were excellent for CR1 patients; 87 and 75%, also good for CR2; 46 and 43 %, and still acceptable for CR3 or advance disease group; 30% for both. In the CR2 group there were 4 late relapses at 19, 24, 27 and 37 months post transplant. Fig 1
Conclusion
This study included only patients younger than 18 years with high risk leukemia transplanted with haplo PBSC and with PTCy. After a follow up of 26 months for surviving patients, the OS is outstanding for patients in CR1, encouraging for CR2 and satisfactory for advance disease, the TRM is not high and the overall incidence of acute and chronic GVHD acceptable, this confirm the value of this procedure in the population studied. However late relapsed occurred and we noticed, similar to an Indian report, (Biol Blood Marrow Transplant 2016; 22:499) a high incidence of severe aGVHD in children < 10 years, it seem that this group may needs innovative approaches for the prevention of this complication
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal